Fibromyalgia
Fibromyalgia
What is Fibromyalgia Syndrome?
FMS (Fibromyalgia Syndrome) is a widespread musculoskeletal pain and fatigue disorder for which the cause is still unknown. Fibromyalgia means chronic and widespread pain in the muscles, ligaments, tendons and the soft fibrous tissues in the body.
Most patients with FMS say that they ache all over. Their muscles may feel like they have been pulled or overworked. Sometimes the muscles twitch and at other times they burn. More women than men are afflicted with FMS, and it shows up on people of all ages. The usual patient is a middle-aged woman.
In addition, they feel devoid of energy as though someone had unplugged their power supply. While the severity of symptoms fluctuates from person to person, FMS may resemble a post-viral state.
It is not a depressive or psychiatric illness, though psychological stress can worsen it.
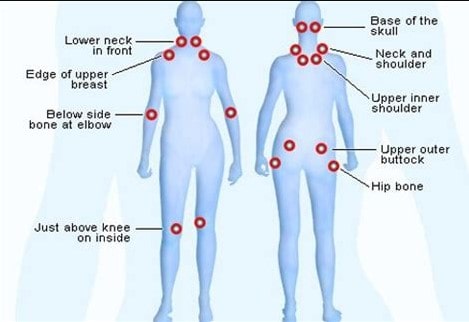
Symptoms and associated syndromes pain: The pain of FMS has no boundaries. People describe the pain as deep muscular aching, throbbing, shooting, and stabbing. Intense burning may also be present. Quite often, the pain and stiffness are worse in the morning and it may hurt more in muscle groups that are used repeatedly.
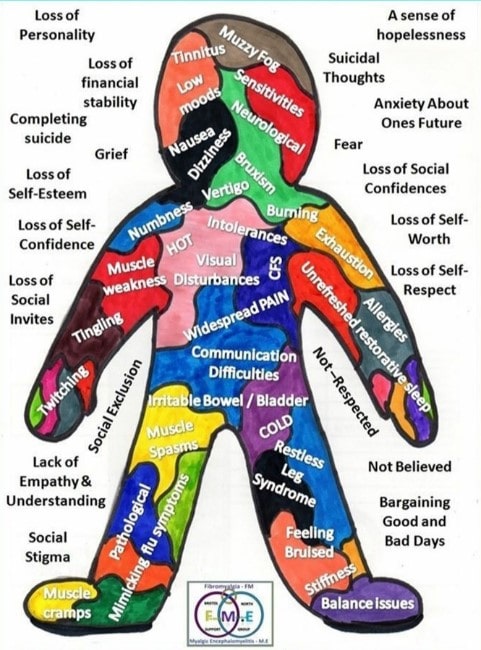
Fatigue: This symptom can be mild in some patients and yet incapacitating in others. The fatigue has been described as “brain fatigue” in which patients feel totally drained of energy. Many patients depict this situation by saying that they feel as though their arms and legs are tied to concrete blocks, and they have difficulty concentrating, e.g. brain fog.
Sleep disorder: Most FMS patients have an associated sleep disorder called the alpha EEG
anomaly. Researchers found that most FMS patients could fall asleep without much trouble, but their deep level (or stage 4) sleep was constantly interrupted by bursts of awake like brain activity. They have more rapid eye movement or REM sleep (full of dreams & yet like awake state) & less of slow-wave (restful) sleep.
Irritable Bowel Syndrome: Constipation, diarrhea, frequent abdominal pain, abdominal gas, and nausea represent symptoms frequently found in roughly 40 to 70% of FMS patients.
Chronic headaches: Recurrent migraine or tension-type headaches are seen in about 50% of FMS patients and can pose a major problem.
Temperomandibular Joint Dysfunction Syndrome This syndrome, sometimes referred to as TMD, causes tremendous jaw-related face and head pain in one-quarter of FMS patients. Typically, the problems are related to the muscles and ligaments surrounding the jaw joint and not necessarily the joint itself.
Other common symptoms: Premenstrual syndrome and painful periods, chest pain, morning stiffness, cognitive or memory impairment, numbness, and tingling sensations, muscle twitching, irritable bladder, the feeling of swollen extremities, skin sensitivities, dry eyes and mouth, dizziness, and impaired coordination can occur. Patients are often sensitive to odors, loud noises, bright lights, and sometimes even the medications that they are prescribed. In fact, FMS is now part of a spectrum of disorders called ‘ CENTRAL SENSITISATION DISORDER’ which encompasses all forms of chronic pain disorders like chronic fatigue syndrome, myofacial pain syndrome/repetitive strain injury/ Irritable bowel syndrome & Premenstrual tension, etc.
Aggravating Factors: Changes in weather, cold or drafty environments, infections, allergies, hormonal fluctuations (premenstrual and menopausal states), stress, depression, anxiety, and over-exertion may all Contribute to symptom flare-ups.
Possible Causes: The cause of FMS remains: elusive, but there are many triggering events thought to precipitate its onset. A few examples: would be an infection (viral or bacterial), an automobile accident or the development of another disorder, such as rheumatoid arthritis, lupus Sjogren’s syndrome or hypothyroidism. These triggering events probably don’t cause FMS, but rather, they may awaken an underlying physiological abnormality that is already present Deranged levels of substance P (elevated) and serotonin (reduced) is a likely cause. Normally substance P is pain-producing & serotonin is sleep-inducing chemicals in brain
Common treatments: Traditional treatments are geared toward improving the quality of sleep and reducing pain. Deep level (stage 4) sleep is crucial for many body functions (Such as tissue repair, antibody production, and the regulation of various neurotransmitters, hormones, and immune system chemicals). Therefore, the sleep disorders that frequently occur in FMS patients are treated first, because they may be a strong contributing factor to the symptoms of this condition.
In addition to medications, most patients may need to use other treatment methods as well, such as physical therapy, occupational therapy, relaxation/biofeedback techniques, manipulation, therapeutic massage, or a gentle exercise program. Yoga, meditation, pranayamas also help.
What is the prognosis?
Long term follow-up studies on FMS have shown that it is chronic, but the symptoms may wax and wane. The impact that FMS has on daily living activities, including the ability to work a full-time job, differs among patients. Overall, studies show that FMS may be equally severe as rheumatoid arthritis, but a reassurance that the disease is not life-threatening or deforming goes a long way in long term outcome.
A trained rheumatologist can identify true fibromyalgia & differentiate it from Pseudo Fibromyalgia, depressive/psychiatric illness or manipulating behavior problem for deriving
Social/ other benefits. Fibromyalgia is a true pain disorder & patients feel real pain; they don’t malinger.
