Lupus

Lupus
What is Lupus?
Lupus is a chronic, autoimmune disease that can damage any part of the body (skin,joints, and/or organs inside the body). Chronic means that the signs and symptoms tend to last longer than six weeks and often for many years. In lupus, something goes wrong with the immune system, which is the part of the body that fights off viruses, bacteria, and germs (“foreign invaders,” like the flu). Normally our immune system produces proteins called antibodies that protect the body from these invaders. Autoimmune means the immune system cannot tell the difference between these foreign invaders and the body’s healthy tissues (“auto” means “self”) and creates autoantibodies that attack and destroy healthy tissue. These autoantibodies cause inflammation, pain, and damage in various parts of the body.
Is it curable?
SLE is an “INCURABLE DISEASE”, just like diabetes and hypertension. But with the recent availability of good treatment modality, SLE has very bright outlook as in diabetes and hypertension. With current treatment options, patients may feel ‘as if cured, but only with medications. Cure means normality without any medications & that does not happen in SLE. If you have any such belief, please remove that from mind. This misconcept often make patients stop treatment and get in to life threatening emergency.
What are the causes of Lupus?
Genes
No gene or group of genes has been proven to cause lupus. Lupus does, however, appear in certain families, and when one of two identical twins has lupus, there is an increased chance that the other twin will also develop the disease. These findings, as well as others, strongly suggest that genes are involved in the development of lupus. Although lupus can develop in people with no family history of lupus, there are likely to be other autoimmune diseases in some family members.
Environment
While a person’s genes may increase the chance that he or she will develop lupus, it takes some kind of environmental trigger to set off the illness or to bring on a flare.Examples include:
- ultraviolet rays from the sun
- ultraviolet rays from fluorescent light bulbs
- sulfa drugs, which make a person more sensitive to the sun
- sun-sensitizing tetracycline drugs such as minocycline
- penicillin or other antibiotic drugs
- an infection
- a cold or a viral illness
- exhaustion
- an injury
- emotional stress, such as a divorce, illness, death in the family, or other life complications

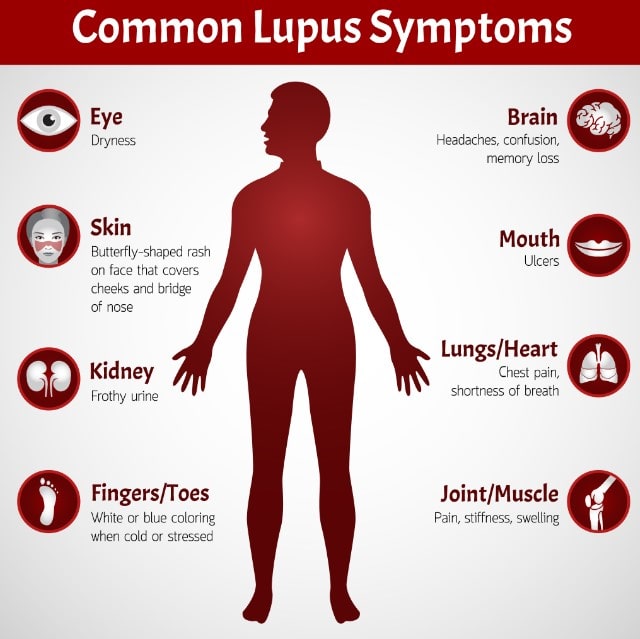
What are the symptoms of Lupus?
Because lupus can affect so many different organs, a wide range of symptoms can occur. These symptoms may come and go, and different symptoms may appear at different times during the course of the disease. The most common symptoms of lupus, which are the same for females and males, are:
- extreme fatigue (tiredness)
- headaches
- painful or swollen joints
- fever
- anemia (low numbers of red blood cells or hemoglobin, or low total blood volume)
- swelling (edema) in feet, legs, hands, and/or around eyes
- pain in chest on deep breathing (pleurisy)
- butterfly-shaped rash across cheeks and nose
- sun- or light-sensitivity (photosensitivity)
- hair loss
- abnormal blood clotting
- mouth or nose ulcers
How is it diagnosed?
Because many symptoms of systemic lupus erythematosus (SLE) mimic those of other illnesses, lupus can be a difficult disease to diagnose. The diagnosis of lupus is based off of a combination of physical symptoms and laboratory results and for most people is not a onetime diagnosis. More often than not it is a diagnosis that evolves over time either towards more certainty that a person does or does not meet the criteria for a diagnosis of lupus.
What treatments are there?
For most people with lupus, proper treatment can minimize symptoms, reduce inflammation and pain, and stop the development of serious organ damage. The information found here will help you understand the most commonly prescribed medicines today, and other drugs under investigation for treating lupus.
Health professionals continue to search for better ways to care for and treat people with lupus. Understanding what causes the disease and why certain people are more likely to develop it may one day lead to promising new treatments for, or even prevention of, lupus. In the meantime, researchers continue to look for new treatments and ways to modify existing ones so they can diminish or eliminate side effects and improve the quality of life for people who have lupus.
Should the patients take the drugs over the counter (OTC)?
No. Steroids have long term side effects. Tapering and monitoring should be done to minimize these effects. Hence care should be taken in not taking these drugs over the counter.
How frequently the doctor should be consulted?
After diagnosis, follow up should be made every month. Once stable the patient should visit the physician at-least once in 3 months. An eye check is a must once in 6 months. Any inter current infection should be treated promptly.
Is there a role for diet restriction?
“No diet can cause or no diet can cure SLE”. But fish can be taken often, as it contains Omega 3 fatty acids, which has an anti-inflammatory effect and also prevents cardiac complications. Restrict saturated fat and high carbohydrate diet. Most Indian spices are beneficial especially curcumin in turmeric.
Is it hereditary?
Most systemic autoimmune diseases have multifactorial etiology and there is a likely hood of the off springs getting SLE or any other connective tissue disorders. But it doesn’t follow any inheritance pattern and often not predictable.
What are the concerns with pregnancy in a SLE patient?
Pregnancy flares up the disease leading to a higher risk of miscarriages due to the presence of Anti-phospholipids antibodies. Pregnancy in SLE need special care as there is risk to the life of both mother and fetus, if not monitored well.
Is there any preventive drug for an SLE patient who becomes pregnant?
No clear evidence in that; directing close monitoring with Rheumatologist/ immunologist and obstetrician is the best option. Blood thinners are also used under supervision.
