Osteoporosis
Osteoporosis
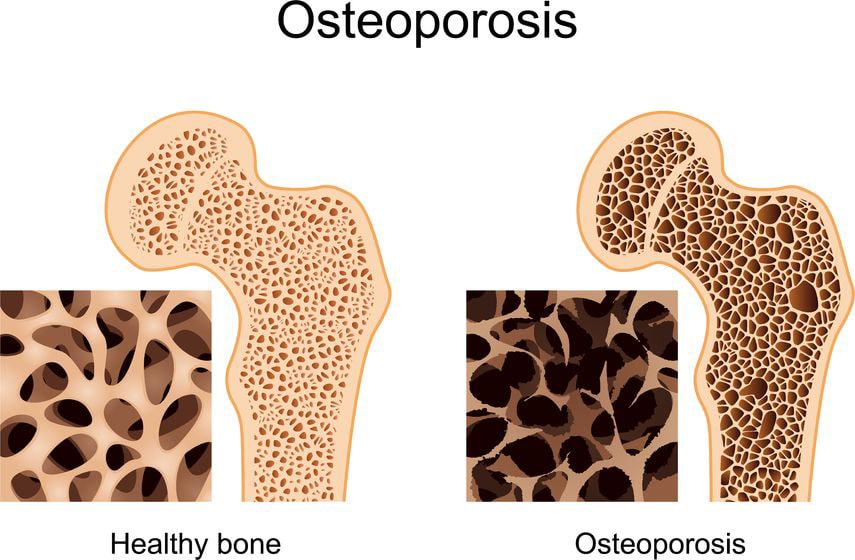
What is Osteoporosis?
The word ‘osteoporosis’ means, literally, ‘porous bone’. It is a condition where you gradually lose bone material so that your bones become more fragile. As a result, they are more likely to break even after a simple fall.
What causes Osteoporosis?
Our bones grow during childhood and adolescence and are at their strongest in the late 20s. As middle age approaches the bones very gradually begin to become weaker. This weakening or thinning of the bones continues as we get older.
The process speeds up in women in the 10 years after the menopause. This is because the ovaries stop producing the female sex hormone estrogen – and estrogen is one of the substances that helps keep bones strong. Men suffer less from osteoporosis because their bones are stronger in the first place and they do not go through the menopause.
What are the symptoms of osteoporosis?
Quite often the first sign of osteoporosis is breaking a bone in a minor fall or accident. Fractures are most likely to happen at the hip, spine or wrist.
Spinal problems occur if the bones in your spine (vertebrae) become weak and lose height (described as a vertebral crush fracture). This usually happens around the middle/lower back. If several vertebrae are affected, your spine will start to curve and you may become shorter. This can sometimes cause back pain and some people may have difficulty breathing simply because there’s less space under their ribs.
People who have spinal fractures will also have a greater risk of hip and wrist fractures. Spinal fractures can even occur without any injury.
Who is at risk?
All of us are at risk of developing osteoporosis as we get older, which is why elderly people are more likely to break bones when they fall. But there are some people who are more at risk of osteoporosis than others. These are some of the factors that can make a difference:
- Steroids If you take prednisolone over a long period
of time, it can lead to osteoporosis. - Oestrogen deficiency Women who have had early menopause (before the age of 45), or a hysterectomy where one or both ovaries have been removed, are at greater risk. Removal of the ovaries only (ovariectomy) is relatively rare but is also associated with an increased risk of osteoporosis.
- Lack of exercise Moderate exercise keeps the bones strong during childhood and throughout adulthood. Anyone who does not exercise, or has an illness or disability which makes exercise difficult, will be more prone to losing calcium from the bones, and so more likely to develop osteoporosis. Exercise is therefore very important in preventing osteoporosis. (However, there is one case in which this is not true: for the small number of people who exercise very intensively, particularly women who exercise so much that their periods stop, the risk of osteoporosis may actually be increased.)
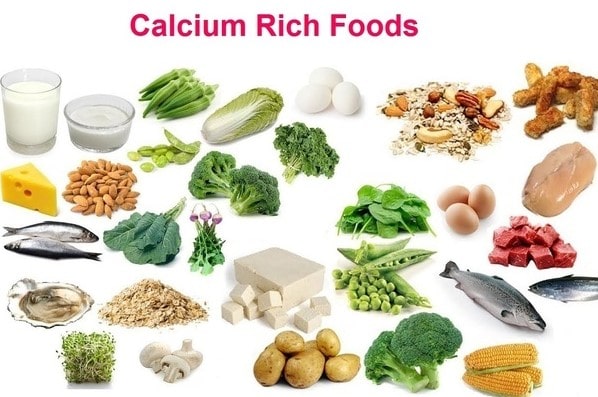
- Poor diet A diet which does not include enough calcium or vitamin D can make osteoporosis more likely
- Heavy smoking Tobacco lowers the oestrogen level in women and may cause early menopause. In men, smoking lowers testosterone activity and this can weaken the bones.
Can you prevent osteoporosis?
There is a great deal which can be done at different stages in your life to guard against the condition.
- Healthy diet Children and adults need a diet which contains the right amount of calcium. The best sources of this are milk, cheese and yogurt and, certain types of fish which are eaten with the bones. If you are watching your weight it’s worth knowing that skimmed or semi-skimmed milk actually contains more calcium than full-fat milk. We recommend a daily intake of calcium of
1000 milligrams (mg) or 1500 mg if you are over 60. A pint of milk a day, together with a reasonable amount of other foods that contain calcium, should be sufficient. Vitamin D is needed for the body to absorb calcium. Vitamin D is produced by the body when sunlight falls on the skin, and it can be obtained from the diet (especially from oily fish) or vitamin supplements For people over 60, it may be helpful to take a supplement containing 10–20 micrograms (µg) of vitamin D. - Children’s exercise Children should actively take part in sports or other types of exercise to help strengthen their bones.
- Adult exercise For the same reason, adults should keep physically active all the way into retirement. Choose ‘weight-bearing’ exercises (any activity which involves walking or running) which are of more benefit for bone strength than non-weight-bearing exercises such as swimming and cycling.
- Smoking Avoid smoking. As previously mentioned, smoking can affect the hormones (in men and women) and may, therefore, increase the risk of osteoporosis.
- Drinking Avoid drinking too much alcohol. The recommended daily maximum for a woman is 2–3 units. For a man, it is 3–4 units. A unit is a single measure of 25 ml of spirits (40% alcohol by volume, or above), or half a pint (0.3 litre) of normal-strength beer, lager or cider (3.5% above), or a very small glass (no more than 85 ml) of wine (12% abv).
What treatments are there?
Apart from the preventative measures already described there are other treatments available if you have osteoporosis. These may slow down the loss of bone or reduce the risk of fractures.
- Calcium and vitamin D As mentioned earlier, people over 60 may benefit from taking small daily amounts of vitamin D, along with 1500 mg of calcium. Stronger vitamin D preparations are sometimes used to treat osteoporosis in younger people.
- Bisphosphonates This group of drugs works by slowing bone loss in many people, an increase in bone density can be measured over 5 years of treatment. Both alendronate and risedronate reduce the risk of hip and spine fractures in patients with osteoporosis. These drugs cannot be taken with food, and specific instructions on how to take the tablets are provided as they can cause irritation of the gullet. They are available either as daily-dose tablets or weekly-dose tablets.
- Hormone replacement therapy Women who have been through the menopause may consider using hormone replacement therapy to reduce their menopausal symptoms. HRT is only beneficial for bones while it is being used. A very large clinical trial reported in 2002 that using the commonest type of HRT tablet is associated with a reduction in fracture, but also with an increase in the risk of heart disease and breast cancer. It can also increase the risk of venous thrombosis. If you are considering long-term HRT use, discuss the potential risks and benefits with your doctor.
- Selective estrogen receptor modulators (SERMs) As previously mentioned, the hormone estrogen helps to keep the bones strong. Raloxifene is a SERM that mimics this effect and reduces spine fractures. It also reduces the risk of breast cancer without increasing the risk of heart disease. It is taken by mouth once a day without the need to follow special instructions. It may cause side effects like menopausal ‘flushing’ and, as with HRT, may increase the risk of venous thrombosis.
- Calcitonin is a substance which the body produces naturally and which helps keep the bones healthy. When used as a treatment it has enabled the bones of people with osteoporosis to grow stronger. Calcitonin can only be given in the form of an injection or by nasal spray. Injections of calcitonin are normally given only as a short-term treatment for painful vertebral fractures, but the nasal spray may be used as a long-term treatment for osteoporosis. Possible side-effects include hot flushes, nausea, an unpleasant taste in the mouth, tingling in the hands and, rarely, an allergic reaction. The nasal spray may also cause a blocked or runny nose, sneezing and headaches.
- Teriparatide Teriparatide is a new drug that helps new bone to form and therefore reduces the risk of fractures. It is taken by daily injection into the thigh or tummy (patients are shown how to do this themselves). It is used for up to 18 months, during which time the bones are strengthened. At present, it is used mainly for people who have had fractures despite using other treatments, or who have had side-effects from other treatments. Side-effects of teriparatide include nausea, limb pain, headaches, and dizziness, but because it is a new drug the longterm side-effects are not known.
How can osteoporosis be detected?
There are no obvious, physical signs of osteoporosis because no one can see the bones getting ‘thinner’. Osteoporosis can go unnoticed for years without causing any symptoms. Quite often the first indication that someone has a problem is when s/he breaks a bone in what would normally have been a minor accident. Relatively minor fractures of the spinal bones can cause you to become round-shouldered and to lose height. These minor fractures may be painless but can cause back pain in some people.
If a doctor suspects osteoporosis, she or He can order a scan to test the strength or density of the bones. This scan is now available at many hospitals throughout the country. The results will tell how much risk there is of the bones fracturing. You will need to lie on a couch, fully clothed, for about 15 minutes while your bones are x-rayed. The dose of x-rays is tiny – about the same as spending a day out in the sun. The technique is called dual-energy x-ray absorptiometry.



